THE IMPORTANCE OF ENDOMETRIAL RECEPTIVITY
We know that the endometrium is the layer lining the inner wall of the uterus, responsible for allowing the embryo’s implantation in the first instance and then giving rise to the maternal side of the placenta. But do we understand what endometrial receptivity is and its importance in the quest for pregnancy?
We spoke with Maripaz Jiménez Guerrero to learn more. She is specialist in Molecular Biology and biotechnology. Besides being passionate about nature, she is immersed in her thesison the application of molecular techniques in endometrial receptivity.

According to Maripaz, throughout our menstrual cycle, the endometrium changes in response to hormonal signals (mainly progesterone and estrogen). These processes are well synchronized with what happens in the ovary, but there is also precise and dynamic communication between various systems and this tissue. Therefore, endometrial receptivity encompasses all processes that take place in the endometrium, favoring the implantation and development of the embryo.
To achieve a successful pregnancy, a quality embryo, proper endometrial receptivity, and good communication between both are necessary. The implantation window is the period during which this dynamic process occurs.
Can endometrial receptivity be assessed?
The short answer is Yes. Understanding the phases of the process or the involved elements helps establish criteria for evaluating endometrial receptivity.
Gynecologists use various techniques to assess endometrial receptivity and increase the chances of achieving pregnancy in an in vitro fertilization cycle. For example, receptivity tests are commonly used to determine if there is a shift in the implantation window that requires changes in hormonal treatment or embryo transfer guidelines.
Some techniques used to evaluate endometrial receptivity include:
- Transvaginal ultrasound and Doppler ultrasound to measure endometrial thickness. The most noticeable change in a receptive endometrium is an increase in thickness due to vascularization, the creation, and remodeling of new blood vessels. If you are undergoing assisted reproduction treatment, especially during the embryo transfer process, you may have noticed the importance placed on endometrial thickness in ultrasound checks.
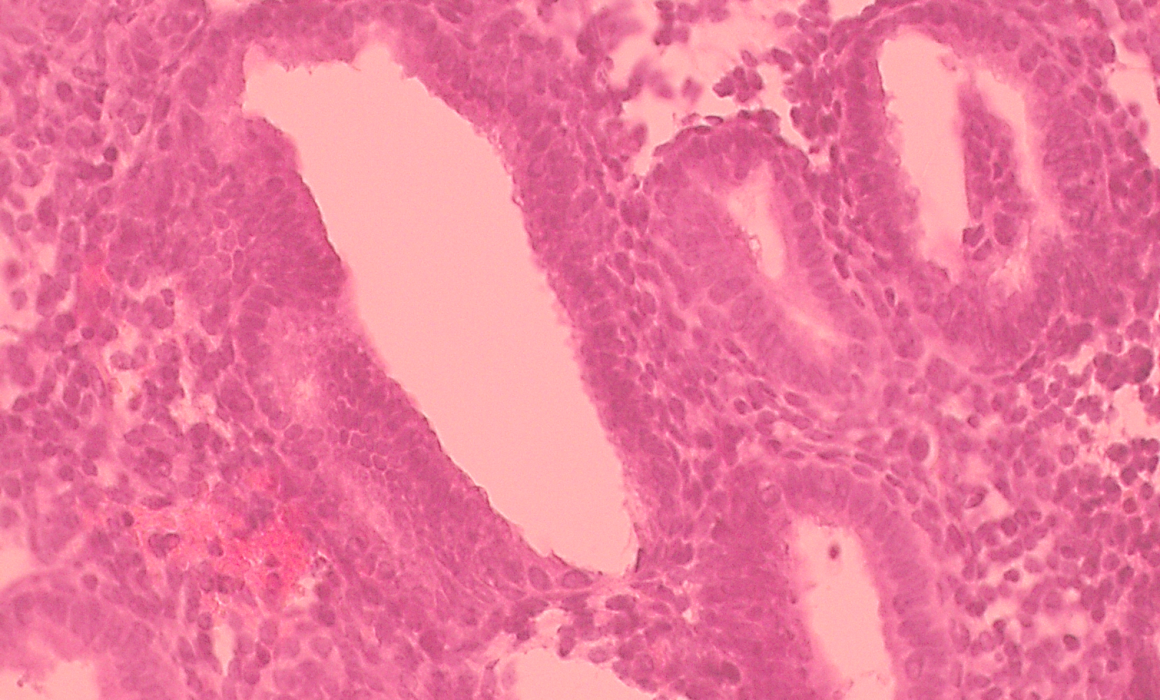
- Endometrial biopsy to study the changes that endometrial cells undergo throughout the menstrual cycle to adapt to the needs of both implantation and embryo development.
- Endometrial biopsy to study the gene profile being expressed in the tissue at the optimal moment for embryo implantation. These genes give rise to a message that tells the cells how to behave or transform. If any message doesn’t reach, is overexpressed, or is not produced, the endometrium may not be ready for implantation when the embryo is presented.
- Hormonal tests that measure the levels of certain hormones in the blood to determine which phase of the cycle we are in or if it is affecting the cycle.
- Other more specific and innovative tests to evaluate specific cells, such as immune system cells specific to the endometrium, or the microbiota, which seems essential not only for our life but also for achieving a healthy pregnancy.
For those who may not know, the microbiota is the set of microorganisms that coexist in our bodies and are essential for our life. According to recent studies, it also seems crucial for achieving a healthy pregnancy.
The assessment of endometrial receptivity, as well as the technique used (because not all are equally invasive, and access to all may not always be available), depends on each case.
Can I improve my endometrial receptivity?
Endometrial receptivity is part of a complex and communicative process whose ultimate goal is pregnancy.
In general, maintaining a healthy lifestyle, with a balanced diet respecting our microbiota, engaging in physical exercise, and avoiding the consumption of processed foods, alcohol, tobacco, and sugary or caffeinated beverages, promotes a healthy menstrual cycle. It is also important to manage stress, respect sleep and rest schedules, and take care of mental health.
Determining the presence of pathological causes that may interfere with endometrial receptivity is crucial. Conditions such as polycystic ovary syndrome (PCOS), endometriosis, hormonal imbalances, dysbiosis (imbalance in the microbiota), obesity, anorexia, diabetes, and autoimmune diseases directly impact fertility. In this context, assessment and follow-up by a clinical professional are indispensable.
Other factors that may also affect include anatomical factors (physical malformations in the fallopian tubes or uterus, or scars from previous surgeries); immunological factors, such as autoimmune diseases or endometritis (inflammation of the endometrium caused by bacterial infection, generally); or advanced age.
Although we cannot reverse aging, ruling out a diagnosis of pathological or anatomical cause and adopting healthy lifestyle patterns promote the smooth operation of our reproductive, endocrine, and immune systems. This ensures that all molecular signals function, the tissue acquires the appropriate thickness with the necessary blood vessels, and the immune and microbiological environment is suitable for developing a healthy pregnancy.
In summary, according to Maripaz, thanks to advances in science, increasingly precise techniques are being incorporated, providing more information for the assessment of endometrial receptivity.
In addition to understanding the entire process in detail, new studies also allow the selection of less invasive markers (molecules or techniques) that do not require endometrial biopsies. Together, they bring us closer to what truly increases the chances of achieving pregnancy: personalizing assisted reproduction treatment for each woman.
Do you have any questions about endometrial receptivity? Feel free to contact me. 😉